Tag: west Africa
Filter by:
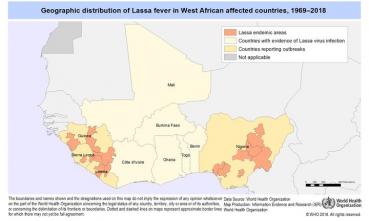
Lassa Fever Outbreak in Nigeria

A few years ago, West Africa was struck by an epidemic of Ebola, which killed more than ten thousand people in Liberia, Sierra Leone, and…
Are Fears of a Global Ebola Pandemic Warranted?

Ebola is a hot topic in the media right now, with multiple cases being reported outside of West Africa and much confusion among the general…
Assessing the Risk of a Global Ebola Pandemic

With the current outbreak of Ebola in western Africa, as well as the recent MERS coronavirus and H7N9 avian flu outbreaks, the world is…