Tag: pandemic
Filter by:
New, More Transmissible U.K. Variant of SARS-CoV-2

While England was enduring its second lockdown during November 2020, and with the other three countries within the United Kingdom following…
The Coronavirus Outbreak: Part One – Modeling “S...

Since 2017, in modeling the threat from wildfire on communities in California, the significant new RMS innovation has been in capturing the…
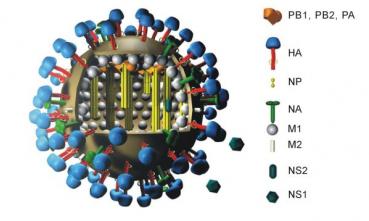
A Coup Against Flu?

Recent articles from two separate research groups published in Science and Nature Medicine report major breakthroughs in flu vaccine research…
Are Fears of a Global Ebola Pandemic Warranted?

Ebola is a hot topic in the media right now, with multiple cases being reported outside of West Africa and much confusion among the general…
Assessing the Risk of a Global Ebola Pandemic

With the current outbreak of Ebola in western Africa, as well as the recent MERS coronavirus and H7N9 avian flu outbreaks, the world is…