With the current outbreak of Ebola in western Africa, as well as the recent MERS coronavirus and H7N9 avian flu outbreaks, the world is becoming increasingly concerned about the risk of emerging infectious diseases and their potential to cause the next pandemic.
As catastrophe modelers, how do we assess the risk of a pandemic?
To understand the potential dangers of Ebola, it’s helpful to look to the framework we use at RMS to model infectious disease pandemics. The RMS® LifeRisks Infectious Disease Model projects the excess mortality risk for existing infectious diseases, like influenza, as well as infectious diseases that are emerging or have recently appeared, like Ebola. When modeling a disease, we first look at two main criteria: the virulence and the transmissibility of the pathogen responsible for causing the disease. We then take into account mitigating criteria, including medical and non-medical interventions.
Virulence
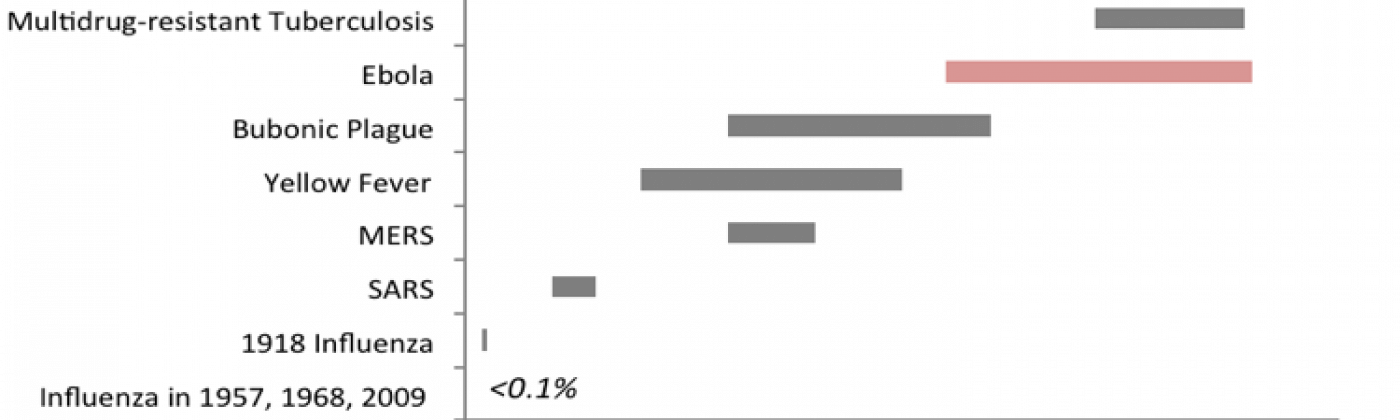
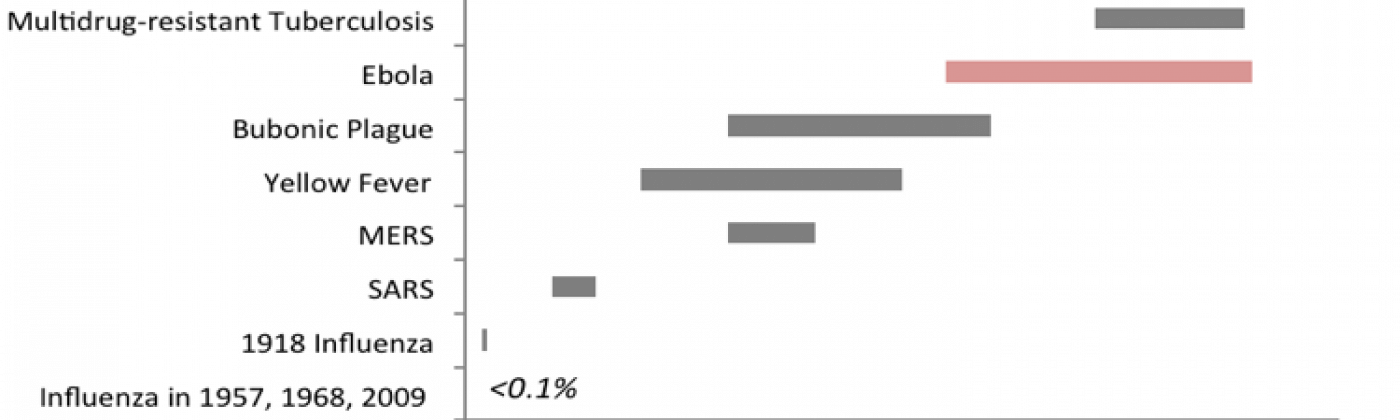
Virulence is a measure of how deadly a disease is, typically measured by the case-fatality rate (CFR), which is the proportion of people who die from the disease to those who do not. The current Ebola CFR is 55 percent. For comparison, the CFR for bubonic plague typically ranges from 25 to 60 percent. CFR for flu is typically less than 0.1 percent.
Transmissibility
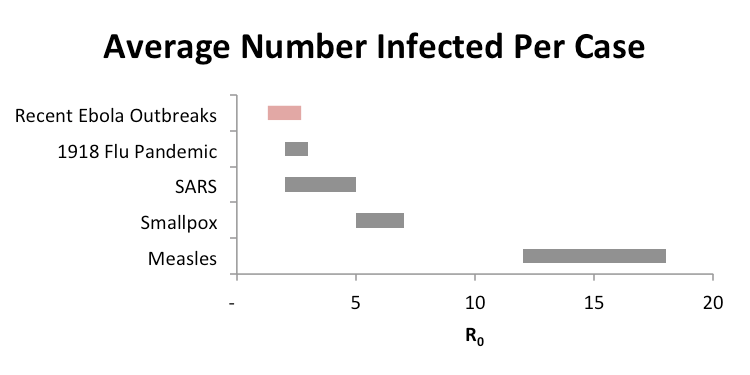
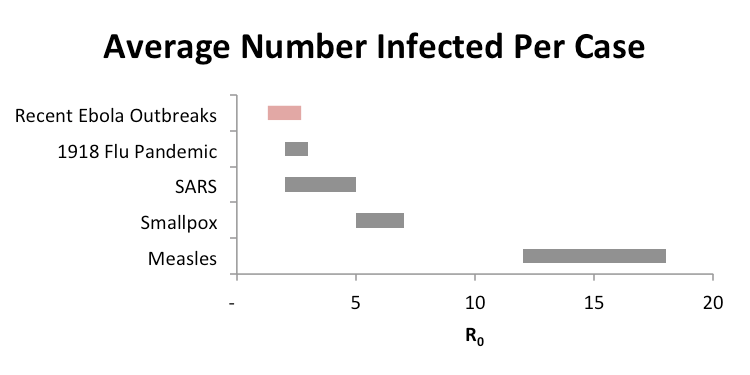
Transmissibility refers to how likely an infected person is to transmit the disease to another person, and is measured in terms of the basic reproductive number, or R₀ of infection, which is the average number of additional infections one person generates over the course of illness. In order to cause an epidemic, R₀ needs to be greater than 1.
The R₀ for the current Ebola outbreak is greater than 1, and the disease will continue to spread. Past Ebola outbreaks have been estimated to be in the 1.3 to 1.6 range, but have occasionally been greater than 5, which is why there is cause for concern. However, Ebola is less transmissible than many other infectious diseases. For example, measles, which is highly transmissible, has an R₀ of greater than 10 in an unvaccinated environment.
Societal and Environmental Factors
Societal and environmental factors can play a large role in transmissibility. In this case, societal and environmental factors in West Africa have contributed to the disease’s spread. For example, traditional burial practices in which families wash the deceased can expose additional people to the virus.
However, the risk of Ebola developing into a pandemic that extends beyond the region is low, due to the standard public health and infection control practices in place in many countries globally. Ebola can only be transmitted via direct contact with bodily fluids, especially blood, which means that caregivers are the primary people who might be exposed to the virus. In many countries including the U.S., the general practice is to treat all blood as potential sources of infection, due to experience with HIV and other blood-borne diseases. In quarantine situations, such as those being used with the American Ebola cases in Atlanta, the likelihood of transmission from a single person is miniscule.
Medical and Non-Medical Interventions
Medical and non-medical interventions mitigate the risk of an infectious disease pandemic. Typical medical interventions for infectious disease include pharmaceuticals and vaccines. Often, there is no specific therapy or drug available for new or emerging diseases. In these cases, we model the effect of supportive care, which includes management of blood pressure, oxygen, and fluid levels. As we’ve seen with the current outbreak, supportive care and the access to healthcare can vary substantially, depending on the region or population. With the exception of experimental treatments, there are no pharmaceutical interventions available for Ebola. Experimental Ebola drugs are not applicable to large populations at this time.
If there are high enough immunization rates, vaccines can reduce or stop the spread of diseases like measles or whooping cough. Unfortunately, a vaccine isn’t currently available for Ebola. Ebola outbreaks occur sporadically and are caused by different virus strains, making vaccine development more difficult.
In addition to vaccines and medical interventions, we account for non-medical interventions when modeling the impact of pandemics. Non-medical interventions include quarantines, school closures, and travel restrictions. Various countries in Africa have begun to implement these methods in hopes of stopping the spread of Ebola. However, these types of countermeasures can often be difficult to time or enforce properly. Ebola can have an incubation period from two days to as long as 21 days.
So, what is the pandemic potential of Ebola?
The current outbreak is now the largest outbreak of Ebola to date, and the World Health Organization (WHO) has designated the outbreak as a Public Health Emergency of International Concern. However, while cases will continue to develop, a global pandemic is unlikely. Even if the disease were to spread to other regions of the world, Ebola is still considered a rare disease and the transmissibility is likely to be much lower due to quarantine and infection-control measures, even if the CFR remains high. We have not seen any community transmission outside of Africa, and this is expected to continue. Ebola is a very serious disease, with devastating consequences to impacted communities. As risk managers, we aim to improve understanding of catastrophes such as pandemic disease so that as a society we can be better prepared to mitigate risk and recover from catastrophes.
Rebecca Vessenes contributed to this post. As a Senior Quantitative Modeler at RMS, Rebecca is involved in the development and parameterization of the LifeRisks longevity models. She recently completed the longevity model for Japan and has worked on determining the correlation structure for mortality improvement between countries. Prior to working for RMS, she led the Financial Modeling group at AIR. Rebecca earned a Ph.D. in mathematics from California Institute of Technology and is an actuary with the Society of Actuaries.